
www.meucare.com
FOR IMMEDIATE RELEASE
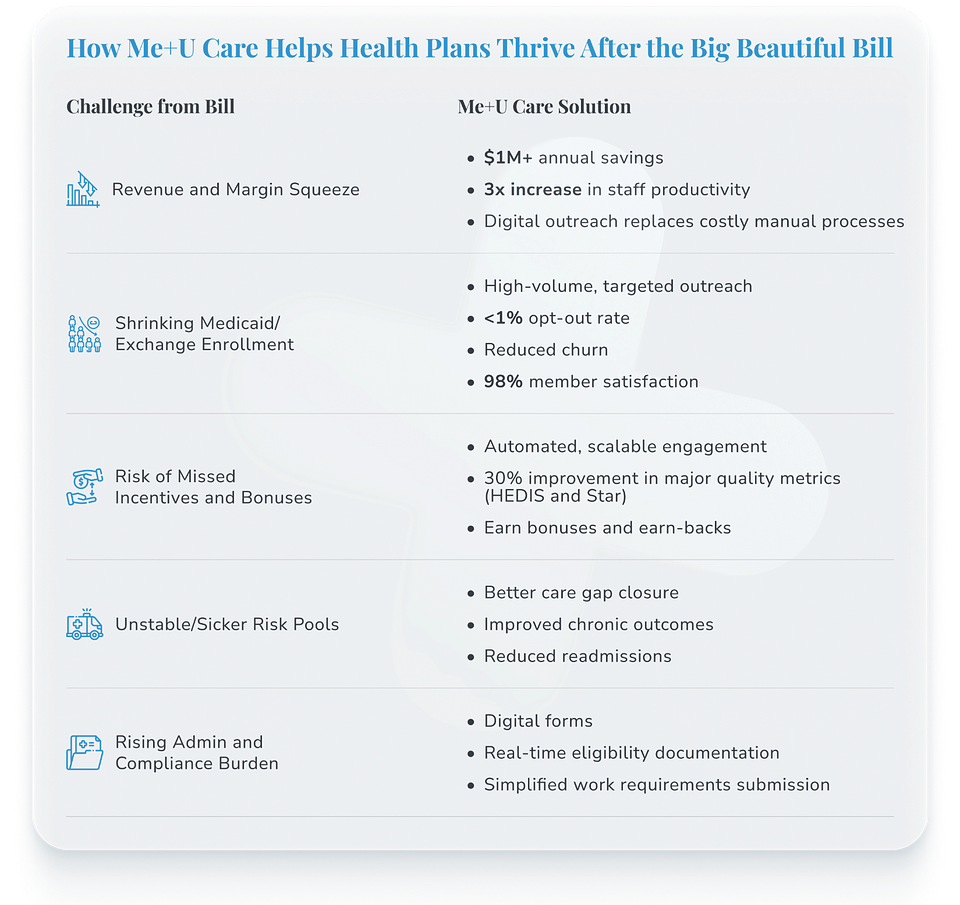
Surviving the Triple Threat: How Health Insurers Can Adapt to the Big Beautiful Bill With Me+U Care
As the Big Beautiful Bill disrupts payer strategy, Me+U Care’s member engagement platform helps plans immediately tackle cost pressures, meet quality measures, and close care gaps.
July 17, 2025 – The “Big Beautiful Bill” has altered the health insurance landscape. Insurers face pressures that could lead to a jump in out-of-pocket health costs for Americans, representing a triple threat to the health plans:
1. Cuts to Medicaid;
2. Federal policy changes that will hit the ACA Marketplace enrollment; and
3. Medical costs rising faster than expected.
Insurers now face a shrinking customer base and mounting operational challenges. In this uncertain environment, Me+U Care emerges as a personalized communication platform that helps insurers retain more members, drive member action, and close care gaps.
Demonstrating 92% member reach without apps, logins, or portals, 98% user satisfaction, and up to 30% improvement across quality measures, Me+U Care enables insurers to sustain revenues, optimize FTE and operational costs, and maintain competitiveness.
Simplifying Workplace Requirements Compliance and Eligibility
Administrative pressure is mounting as eligibility redeterminations and documentation requirements become more frequent. Me+U Care’s digital-first tools keep members covered and plans compliant with minimal lift, without the need for members to download an app or navigate websites.
The bill states that by the end of 2026, plans are required to inform Medicaid enrollees about work requirements as well as how to comply. A notice “shall be delivered” by mail or email and in an additional form. Those additional options include a phone call, text message, a website, “other commonly available electronic means,” or “other forms as the Secretary deems appropriate.”
· Streamlined Documentation: Me+U Care’s ability to digitize workplace requirement documentation, coupled with e-Sign capabilities automates and simplifies compliance with new, more frequent eligibility reviews, reducing the cost and workload associated with increased administrative complexity.
· Boosting Compliance Rates: With a member opt-out rate less than 1%, instant digital delivery via SMS allows real-time responses, facilitating continuous coverage for eligible members and mitigating enrollment "churn."
Navigating Reduced Enrollment with Me+U Care
· Targeted Member Engagement: As Medicaid rolls and Marketplace participation decline, insurers must maximize retention and outreach to every remaining member. Me+U Care enables plans to send millions of messages using just part-time staff, ensuring vital communications reach at-risk members, including those facing coverage loss.
· Digital "Find a Number" Service: For members with outdated or missing contact information (especially in Duals populations), Me+U Care’s unique “find a number” service has shown a 66% success rate, turning unreachable members into active participants.
However, shrinking enrollment isn’t the only pressure. Even among retained members, the rising cost of care and lower reimbursement rates are squeezing margins across the board.
Responding to Revenue & Margin Pressure
· Cost Reduction Through Digitization: The platform digitizes forms and outreach, helping plans save over $1 million annually and offsetting new revenue shortfalls caused by legislative changes.
· Lower FTE and Medical Expenses: With Me+U Care’s scalable app-free Chat and Family Caregiver Network, clients have reported a 3x increase in productivity over phone outreach, directly lowering administrative and care management costs while improving outcomes.
Maximizing Incentive and Earn-Back Revenue
As incentives and bonus structures tighten, payers need streamlined solutions that move the needle on performance without additional overhead. Me+U Care turns digital outreach into dollars earned.
· Enhanced Performance Metrics: Me+U Care’s ability to mobilize family caregivers and automate outreach directly feeds into improved HEDIS and STAR ratings, allowing insurers to capture more federal/state incentives, which are vital as premium subsidies are rolled back.
· Productivity for Fewer Staff: The platform empowers health plans’ Care Managers to increase their workload by 3x with higher efficacy, supporting both cost containment and revenue amplification even with limited personnel resources.
Countering Adverse Selection and Risk Pool Deterioration
A worsening risk pool threatens both financial stability and member outcomes. Me+U Care helps plans stay ahead of high-cost claims by closing gaps faster and keeping chronic conditions in check.
· Care Gap Closure: Proactive, targeted engagement through Me+U Care helps close care gaps at a 2.5x rate even as overall membership declines, which is critical to maintaining quality metrics in sicker risk pools.
· Improved Care Outcomes: Enhanced digital member engagement supports medication adherence, chronic condition management, and a 25% reduction in readmissions, minimizing high-cost claims that are likely to rise as risk pool quality worsens.
The Future of Member Engagement Starts Here
The health plans best positioned to weather the effects of the Big Beautiful Bill are those willing to rethink the infrastructure behind outreach, action, and outcomes. Me+U Care offers a foundation for scalable change, one that aligns operational priorities with member needs and can be implemented in under 30 days without IT integration.
“In the wake of the Big Beautiful Bill, health insurers must innovate to survive and thrive. Me+U Care stands out as a future-ready, efficiency-driving platform, cutting costs, safeguarding revenue, improving quality, and ensuring operational resilience,” says Kendall Lockhart, Founder and CEO of Me+U Care. “By strategically adopting Me+U Care, payers can effectively manage the Bill’s disruptive impacts and continue delivering value to members, providers, and stakeholders.”
The road ahead is challenging, but it’s not insurmountable. For payers ready to lead, this is the perfect opportunity to rethink how member engagement is done with Me+U Care.
Health plans interested in learning more can visit www.meucare.com or email Jay Sebaugh (jay@meucare.com) or Tony Pilotto (tony@meucare.com).
About Me+U Care
Me+U Care is a leading digital-first healthcare communications and outcomes platform, trusted by health plans across the country to deliver better member engagement, lower administrative costs, and measurable improvements in quality and satisfaction. With a focus on seamless, app-free communication and actionable analytics, Me+U Care is redefining what’s possible in healthcare connectivity.
###
For media inquiries, please contact:
press@meucare.com